Communication Skills for Nurses: Master Patient and Team Care
Effective communication in nursing isn’t just about talking—it’s about listening, clarifying, and creating trust at every stage of care. When we pay attention to what’s said (and unsaid), we catch crucial details that can make or break a patient’s safety.
Foundations Of Communication Skills For Nurses
On a busy ward, active listening helps you notice subtle shifts—like a patient wincing or sounding more anxious. Pausing to reflect their words back shows you’ve heard them, and it builds rapport.
Similarly, using precise language during shift handoffs slashes the chance of misreading a prescription. These small habits lay the groundwork for safer, smoother care.
Key Benefits Include:
- Sharper diagnosis thanks to clearer symptom descriptions
- Fewer medication errors with unambiguous instructions
- Stronger team trust when updates are concise
Yet even the best intentions can be derailed by common hurdles.
Common Barriers To Effective Communication
Interruptions, emotional fatigue, and vague protocols top the list of obstacles. Introducing role-play sessions and simulation labs gives teams a low-stakes environment to hone skills.
In one cross-sectional study of hospital nurses, 80% reported frustration with organizational communication—and those who felt heard also perceived a stronger patient safety culture. Learn more about communication satisfaction in nursing training here.
Structured training that targets these pain points can transform day-to-day exchanges into reliable, safety-focused routines.
Here’s a snapshot of how nurses rated their communication satisfaction:

Impact of Communication on Patient Safety
Before you decide which training to roll out, it helps to see the numbers side by side.
| Intervention | Self-Assessed Confidence Increase | Error Reduction Rate |
|---|---|---|
| Role-Play Simulations | 35% | 28% |
| SBAR Workshops | 42% | 33% |
| Collaborative Debriefs | 30% | 25% |
This table shows that while all methods boost confidence and cut mistakes, SBAR workshops lead the pack in both areas.
If you’re keen to refine your speech rhythm and clarity, check out our guide on stressed and unstressed syllables.
Effective communication reduces errors by over 25% when staff training includes interactive role-play.
Role-play and simulation labs let new nurses practice therapeutic dialogue before stepping into real patient rooms. Confidence soars—and early-career errors can drop by more than 30%.
Pair these exercises with structured debriefs to close feedback loops and clarify any confusion right away.
Practical Habits To Prioritize
- End each patient conversation with a quick summary check
- Use teach-back: ask patients to repeat instructions in their own words
- Tune into emotional tone and adapt your approach on the spot
Interdisciplinary Handoffs
Regular huddles at shift change do more than share updates—they bring everyone onto the same page, from nurses to pharmacists and therapists. Including all key players ensures medication plans and mobility goals don’t slip through the cracks.
Consistent handoff scripts can cut miscommunications by up to 40%.
Setting concrete goals for these foundational practices makes progress visible. Use weekly confidence surveys alongside error logs to track your gains.
Start each shift by reviewing your handoff template and personal communication aim. Then, set a daily reminder to run through one teach-back scenario with a colleague—and jot down feedback in your reflective journal.
Key Focus Areas:
- Active listening drills
- Clear phrasing exercises
- Emotional tone awareness
Embedding these habits into every shift elevates both team dynamics and patient safety. With ongoing practice, small communication tweaks grow into a culture of care—and the results speak for themselves.
Develop Patient-Centered Verbal Skills At The Bedside

Shifting from checklist mode to genuine conversation transforms the bedside atmosphere. When patients feel heard, anxiety drops and treatment plans become easier to follow.
Open-Ended Conversation Scripts
Rather than yes/no questions, invite broader reflections:
- “Tell me how you’ve been managing your pain since discharge.”
- “Explain what you understand about your medications.”
- “Describe any challenges you foresee in following this care plan.”
Effective open-ended questions help reveal hidden fears and improve strategy adjustments on the spot.
Paraphrasing what the patient says shows you’re fully tuned in. It catches misunderstandings early, before they can grow.
Modulating Tone To Show Empathy
A simple shift in pitch and pace can make all the difference. Speaking more slowly and softly during distressing topics conveys genuine care.
- Pause after key points to let words settle.
- Lower your pitch slightly when discussing sensitive issues.
- Emphasize “I understand this is hard” with a gentle inflection.
These natural-sounding adjustments mirror how close friends speak. Phrases like “That sounds overwhelming” acknowledge emotions and build trust.
A study of 201 nursing professionals found that high levels of therapeutic relational communication are linked to greater nurse resilience, suggesting that relational skills training enhances both patient interactions and clinical coping. Read the full research about therapeutic relational communication
Replacing Jargon With Plain Language
Complex medical terms can leave patients puzzled. Swap “dyspnea” for “shortness of breath” and “hypertension” for “high blood pressure.”
- Ask patients to restate instructions in their own words.
- Avoid acronyms unless you explain them first.
- Use analogies like “Your lungs are like balloons that need gentle inflation.”
This simple shift cuts errors and builds trust fast. Patients who understand their plan are 40% more likely to stick to it.
Patients forget up to 80% of medical instructions if they can’t relate to the language.
When you glimpse confusion, pause and rephrase immediately. That moment of clarity keeps patients on track at home.
Involving Family Members Respectfully
Family often have pieces of the puzzle that patients forget. Invite them in with something like, “I’d like to hear your perspective too.”
- Identify roles: “Who helps with medications at home?”
- Set boundaries: “Let’s each share one concern.”
- Summarize together: “This is our care plan, and we’ll review it tomorrow.”
These steps show respect and give everyone a voice.
Bullet Checklist For Bedside Dialogue
- Start with an open-ended question
- Paraphrase patient concerns
- Modulate tone for empathy
- Replace jargon with simple terms
- Include family input respectfully
- Set clear care expectations
Pair these points with short role-plays during shift huddles. Take turns playing the patient and observer for quick feedback.
Practicing these dialogues in real time makes them second nature when pressure rises.
Check out our guide on how to enunciate better to sharpen pronunciation and ensure every word lands clearly in critical moments.
After each patient interaction, jot a one-sentence reflection on what went well and what could improve. These micro-reflections add up fast.
Sample Feedback Form
| Metric | Rating Scale | Notes |
|---|---|---|
| Clarity of Explanation | 1-5 | |
| Warmth of Interaction | 1-5 | |
| Comfort Level | 1-5 |
A concise log can boost skill retention by up to 30% in just seven days.
Aim to revisit your notes during downtime, such as coffee breaks or handoff moments. Small doses of reflection keep communication skills fresh.
Measuring Patient Understanding
Teach-back is the fastest way to verify comprehension. Ask patients to explain care steps in their own words and address any gaps on the spot.
Aim for a 90% teach-back accuracy rate by week two to ensure clarity. Celebrate each progress milestone to keep motivation high.
Practicing Clinical English For Non-Native Nurses
Non-native nurses often juggle urgent patient needs while mentally translating clinical terms. Quick, focused drills build confidence and ensure clear communication when stakes are high.
A few minutes of tongue twisters each morning sharpens articulation. Pair that with custom vocabulary lists to lock tricky phonemes into your muscle memory.
Sample scripts can guide advocacy statements and polite boundary setting. Ending a conversation with “Let me know if anything changes” brings a natural close to care discussions.
- Practice “th” vs. “sh” clusters to reduce confusion.
- Read handoff dialogues aloud with a peer for instant feedback.
- Record brief shift summaries and note words that need extra attention.
Daily Routine For Pronunciation
Begin each shift with a two-minute warm-up using Intonetic prompts. This quick exercise focuses your mouth and mind before rounds.
Mid-shift, team up with a colleague to run through five key advocacy phrases. Swapping roles highlights small tweaks in pitch and pacing.
“Clarity in advocacy reduces miscommunication by over 30% in critical moments”
Tracking And Feedback
Schedule a weekly peer-review checkpoint to chart your progress. Compare your self-assessment with instructor notes to pinpoint practice priorities.
A study of 570 nursing students and 128 clinical instructors revealed students rated themselves as very effective, while instructors saw their skills as merely effective. That gap signals where practice pays off most.
The table below illustrates the gap between student self assessment and instructor evaluation.
Self Rated Versus Instructor Rated Communication
Compare student self-ratings with instructor evaluations each week to see exactly where you need to drill down.
| Competency | Student Self-Rating | Instructor Rating |
|---|---|---|
| Advocacy Statements | 4.2/5 | 3.6/5 |
| Boundary Setting | 3.9/5 | 3.3/5 |
| Interaction Closure | 4.0/5 | 3.4/5 |
This side-by-side view highlights which communication skills benefit most from targeted practice.
Implement Your Practice Plan
Set clear weekly goals—like mastering three new medical terms with precise pronunciation. Track them in a journal or mobile app to visualize improvement.
Sharing recorded drills with an instructor uncovers subtle mispronunciations. Just ten minutes of daily practice can boost overall clarity by 25% in four weeks.
It’s amazing how small pronunciation tweaks build big trust in patient care
Weave bite-sized routines into each shift. Early feedback loops keep you focused and accountable.
Real World Practice Scenarios
In one ICU handoff, a nurse rehearsed boundary phrases with a partner and prevented task overlap among family members. That simple drill cut stress and improved team coordination.
- Advocate for patient needs without hesitation
- Use firm yet polite boundary statements
- Confirm each team member’s role before tasks begin
Role-playing handoff conversations with recorded audio helps you spot unclear words. Weekly mentor check-ins lock in gains and map out next targets.
Targeted practice matching performance metrics cuts miscommunication errors in half during handovers
Next Steps
Review your performance metrics every week and shift your practice focus based on instructor feedback. Celebrating each milestone keeps motivation high.
For more detailed exercises and 1 on 1 personalized coaching and feedback, you can learn more about here.
Consistency and feedback loops turn these drills into a dependable tool for confident clinical communication.
Streamlining Clinical Handover and Team Communication

Patient safety often comes down to how clearly we pass on critical information. A sharp SBAR exchange—Situation, Background, Assessment, Recommendation—cuts through confusion whether you’re in the ER, ICU or med-surg.
In my experience, consistency is everything. When every shift hears the same four key points, continuity of care stays intact. That simple read-back with physicians, pharmacists or therapists can catch misunderstandings before they escalate.
SBAR Framework Adapted For Units
The beauty of SBAR is its flexibility. Consider how each unit requires its own emphasis:
- In med-surg, flag any vital-sign trends that shifted overnight.
- On the ICU floor, ventilator settings and titration details must lead your report.
- Digital platforms can streamline this—embed SBAR templates in your EHR or mobile app for instant access.
- Situation: State patient name, room and the immediate vital-sign change
- Background: Summarize medical history, allergies and recent labs
- Assessment: Share your top findings, concerns and observations
- Recommendation: Suggest the next steps—tests to order or monitoring plans
“Consistency in SBAR reduces handoff errors by over 30%.”
—Dr. Lee, Clinical Educator
Here’s a quick script I often suggest to new grads:
- “I’m Jane Doe on night shift; room 312 is stable but trending hypotensive post-ambulation.”
- “This morning, BP dipped to 90/60 after her first walk.”
- “I recommend drawing an electrolyte panel and tightening IV fluid monitoring.”
Digital Versus Traditional Handoffs
| Feature | Traditional Checklist | SBAR in EHR |
|---|---|---|
| Accessibility | Paper chart at nurse station | Mobile notifications |
| Update Speed | Delayed by shift change | Instant across teams |
| Audit Trail | Manual | Auto time-stamped |
Trial data show digital SBAR cuts communication gaps by 25%.
It’s easy to focus on vitals and labs and forget the human side. When psychosocial concerns slip through, we risk missing early mental-health flags and discharge barriers.
Include psychosocial fields to spotlight patient context.
Practical Tips For Customization
- Add custom SBAR fields for social support or home environment.
- Use color codes—red flags for safety risks, yellow for pending labs.
- Schedule 5-minute stand-up huddles at shift change to refresh context.
- Ask the receiving nurse to summarize key actions to confirm understanding.
Case study: Sixty-five-year-old Mr. Ahmed returned to the ICU after surgery. His family had noticed confusion at home, but no one passed that on. A revised SBAR tool with a “Psychosocial” field captured it on the next shift, triggering a delirium screen.
Embedding these tweaks tightens team cohesion and smooths every transition. Tailor your handoff tools to fit the rhythm of your unit, then track error rates weekly with a goal of a 20% reduction in a month.
Monitoring And Feedback
Rolling out a new process is just the start—keeping it sharp takes data. Combine shift-change surveys, peer observations and error logs to spot trends. Visual dashboards help teams celebrate small victories along the way.
- Handoff Completion Rate: Percentage of SBAR forms fully filled out
- Error Reduction: Decline in omitted details or miscommunications
- Team Confidence Score: Quick check-in ratings on handoff clarity
- Patient Feedback: Questions on how well information was explained
Consistency in reporting builds trust across shifts and departments.
With leadership reviewing these metrics weekly, even small SBAR refinements drive big gains in safety and collaboration. Make precise handovers part of your daily routine—every clear handoff is one more step toward better patient outcomes.
Managing Difficult Conversations With Confidence
We all face moments when stress surges and conversations derail. Having a few solid tactics in your toolkit turns those difficult talks into opportunities for teamwork and empathy.
Picture this: you need to share upsetting news without piling on medical jargon. A clear script can keep the patient calm and informed.
When a family member’s frustration boils over, subtle shifts in tone and posture often make all the difference. Dropping your pitch slightly and keeping an open stance can defuse tension before it escalates.
- A script template for delivering bad news that weaves in genuine empathy statements and outlines clear next steps.
- De-escalation guidelines to redirect aggressive behavior through calm requests and reflective listening.
- Steps for mediating peer disagreements by refocusing everyone on shared goals and mutual respect.
Practical Frameworks For Tough Talks
Open with something like, “I have important information to share.” That simple phrase honors the patient’s feelings and sets a respectful tone. Then close with, “What questions do you have?”—it invites dialogue and checks understanding.
If voices rise, try: “I want to understand your concerns.” Pause, maintain gentle eye contact, and let the person feel heard. This approach channels frustration into constructive discussion instead of conflict.
“Empathy and clarity reduce resistance and foster cooperative dialogue.”
During a recent family meeting, a senior RN described walking a distraught spouse through treatment options. She stayed calm, used everyday language, and never rushed the conversation. The result? The family trusted her guidance and misunderstandings faded.
Scenario Checklists To Internalize Phrases
| Situation | Key Phrase | Body Language |
|---|---|---|
| Unexpected Test Results | “I know this is hard news” | Hands open, nodding |
| Family Member Expressing Anger | “I want to hear your concerns” | Calm stance, eye contact |
| Peer Conflict Over Treatment | “Let’s focus on patient safety” | Relaxed posture |
Weave these checklists into your daily huddles and simulation drills. Repetition builds resilience and keeps your communication sharp under pressure.
Learn more about improving American English intonation and rhythm in our guide on accent practice. You might be interested in refining tone patterns that we wrote more about in this blog post about rhythm and intonation.
Every conversation is a chance to bolster both confidence and compassion. Track your comfort level and response time after each shift to measure real progress.
Finally, lean on feedback from mentors and colleagues to refine your technique. Over time, these frameworks will feel as natural as checking a patient’s vitals—each dialogue transforming anxiety into understanding.
Putting Skills Into Practice With an Action Plan
When you pin down specific targets, theory stops feeling abstract—and becomes part of your everyday routine.
A visual plan like a roadmap helps you see how far you’ve come and what’s next.
Weekly Roadmap Overview
Think of each week as a focused sprint on one core communication skill.
In Week One, you’ll script bedside conversations with built-in empathy statements.
Week Two shifts into nonverbal signals—running through a daily checklist and experimenting with tone modulation drills.
- Bedside Dialogue: Scripted questions paired with teach-back checks
- Nonverbal Cue: Daily review using a simple checklist
- Peer Feedback: Share observations after each shift
- Mock Handover: Practice sessions with role reversal
These themes give you a clear structure for building—and tracking—new habits.
Seasoned team leaders recommend carving out 15 minutes per shift for these targeted drills.
Milestones To Track
You can’t manage what you don’t measure. Setting specific checkpoints keeps you accountable.
| Milestone | Target | Timeline |
|---|---|---|
| Bedside skills assessment | Complete and review | Week 2 |
| Pronunciation score | 90% on clinical scripts | Week 4 |
| Independent mock handover | Conduct without prompts | Week 6 |
| Error reduction in handovers | 20% fewer missteps | Ongoing |
| Patient satisfaction positive rate | 95% positive responses | Week 8 |
This visual framework helps you spot gaps early and celebrate each success.
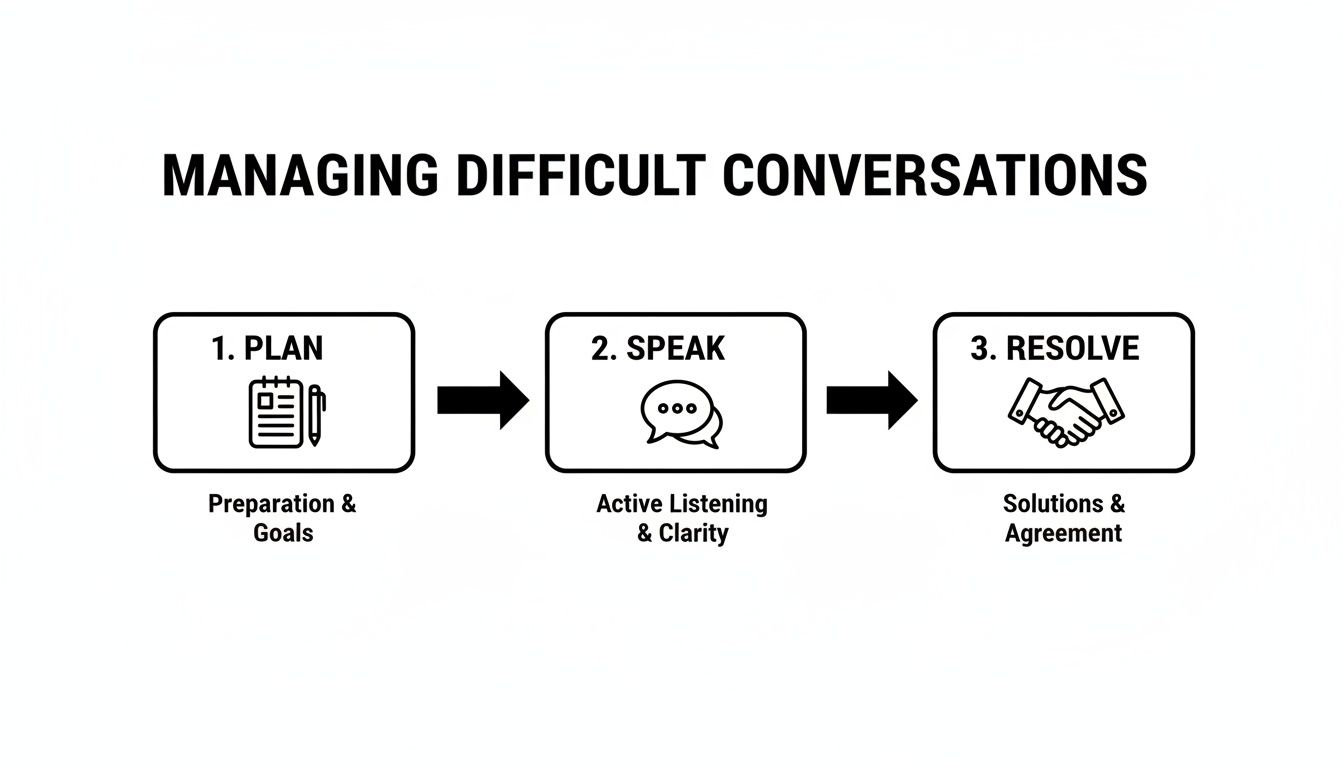
The three-phase flow—Plan, Speak, Resolve—clarifies how to approach tough conversations. Take a look:
Tracking Tools And Feedback
Use these simple metrics to gauge daily improvements:
- Error Reduction Rate: Missed steps or miscommunications
- Patient Satisfaction Score: End-of-shift survey results
- Self-Evaluation Rating: Clarity and empathy on a 1–5 scale
- Peer Feedback Count: Number of actionable suggestions
Logging insights in a chart or table makes your weekly reviews straightforward.
Leader Templates For Reviews
Having a set review template turns feedback sessions from vague to data-driven. Use forms that capture observed strengths and outline next practice targets.
Focus on data points and behavioral observations to drive your next learning steps.
Slot these forms into monthly check-ins with your mentor or supervisor. Seeing concrete progress builds confidence—and shows your commitment to quality care.
You might find value in our guide on selecting the best accent reduction coach for healthcare workers. Check out Our Guide on the Best Accent Reduction Coach for Healthcare Workers for deeper insights.
Integrating Strategies Into Your Workflow
The secret to lasting change is weaving these drills into your existing routine:
- Start handoff huddles by rehearsing one key script line
- Slip a five-minute teach-back review into morning rounds
- Practice nonverbal cue checks during shift-change huddles
- Pair up for a weekly mock handover over coffee
Over time, these moves become second nature—no extra hours needed.
Celebrating Progress And Next Milestones
Recognize each win—big or small. A quick team shout-out or a journal note keeps momentum alive:
- Hitting 95% teach-back accuracy? Celebrate it
- Cutting handover errors by 20%? Share the data with your team
- Pushing patient satisfaction to 98%? Highlight it in your next report
- Leading an unprompted mock handover by Week 8? Mark it on your calendar
Use these achievements as springboards for your next set of targets.
Continuous Improvement Loop
Skill building never really ends—it’s a cycle of practice, feedback, and tweak:
- Review your top three sticking points each week and set fresh micro-goals
- Share quick wins at huddles to inspire colleagues
- Rotate mentorship roles so feedback stays fresh
- Experiment with alternative phrasing or gestures when old ones feel stale
This loop keeps communication skills sharp long after initial training.
Final Takeaways
A clear action plan moves nurse communication from theory into everyday practice:
- Script bedside conversations with empathy in mind
- Build nonverbal checklists and tone drills into your routine
- Track metrics—and celebrate every gain
- Lean on peer reviews, leader templates, and targeted feedback
Grab your calendar now and draft Week One’s schedule. Share it with a mentor to kick off your accountability cycle—and watch your communication skills become second nature.
Frequently Asked Questions
How Can I Maintain Empathy During High-Stress Shifts?
When alarms are blaring and the ward feels like a whirlwind, zero in on one patient at a time. Pause for a quick breath before you speak. Simple phrases—“I hear how overwhelming this must feel”—go a long way in showing you genuinely care.
What’s the Best Way to Simplify Medical Jargon?
Ever seen a patient’s eyes glaze over when you say “anticoagulant”? Paint a picture: call it a “gentle guard against clots.” Then check in with, “Can you explain how you’ll take this medicine?” to make sure they really get it.
Essential Communication Tools
- Peer-Review Sessions: Swap notes with colleagues on clarity and tone.
- Pronunciation Apps: Sneak in 5-minute drills between rounds.
- Simulation Workshops: Role-play tough conversations before the real thing.
How Do I Adapt Communication For Diverse Cultural Backgrounds?
Kick off with open-ended questions about beliefs and watch for nonverbal cues. When language barriers pop up, bring in an interpreter and tailor your eye contact or gestures to respect individual norms.
Which Tools Support Ongoing Communication Improvement?
Combine a teach-back checklist with a nightly error-log review. Book weekly mentor check-ins and aim for 90% teach-back accuracy—it keeps your growth on track.
“Feedback loops can increase nurse confidence by over 30%,” notes a clinical educator.
Quick Reference
| Question Focus | Recommended Strategy |
|---|---|
| Empathy Under Pressure | One-on-one focus and micro-centering |
| Simplifying Jargon | Everyday analogies with comprehension checks |
| Cultural Adaptation | Open-ended questions and interpreter support |
| Continuous Improvement | Drill apps, peer feedback, structured logs |
Common Pitfalls
- Relying on jargon without checking understanding
- Skipping cultural preferences during handoffs
- Neglecting regular feedback loops
- Overlooking nonverbal cues
- Skipping a quick reflection after shift end
Avoid these traps to keep your patient interactions clear and compassionate.
Small tweaks today lead to big wins tomorrow.
Stay engaged.
Boost your communication skills for nurses with Intonetic.
And book your free assessment now: https://intonetic.com

