A Practical Guide on How to Communicate With Patients
Connecting with patients is a delicate dance of clarity, empathy, and trust. It’s more than just knowing the right medical terms; it's about translating that complex knowledge into simple, human language. It’s about truly hearing a patient's concerns and building a rapport that makes them feel safe and understood.
The Critical Link Between Communication and Patient Safety
When a patient walks into your clinic or hospital, they aren't just bringing symptoms. They’re carrying a heavy load of uncertainty, anxiety, and a deep need for reassurance. In this high-stakes world, how you communicate isn’t just a "soft skill"—it's a core component of patient safety and quality care. Every word, your tone, even your body language lays the foundation for their entire experience.
When communication breaks down, the consequences can be devastating. That gap between what you intended to say and what your patient actually understood can lead to medication errors, missed diagnoses, and a complete erosion of the therapeutic relationship.
The Staggering Cost of Miscommunication
The data paints a grim picture. An analysis of over 23,000 medical malpractice lawsuits in the U.S. revealed that more than 7,000 cases were directly linked to communication failures. The financial toll was a staggering $1.7 billion, and even more tragically, these breakdowns contributed to nearly 2,000 preventable deaths.
This isn't an isolated problem. The Joint Commission, a key healthcare accreditation body, has pointed out that communication breakdowns during patient handovers are a factor in as many as 80% of serious medical errors.
When we fail to communicate clearly, we are not just risking confusion; we are risking lives. This reality places an immense responsibility on every healthcare professional to prioritize and master this essential skill.
Unique Challenges for Non-Native English Speakers
If you're a non-native English-speaking healthcare professional, you face an added layer of complexity. Subtle nuances in pronunciation, word stress, and intonation can unintentionally change your message's meaning or the empathy you're trying to convey.
For instance, using a flat intonation while delivering serious news might be interpreted as a lack of concern, even when your intention is purely professional. Mispronouncing a key medical term could, unfortunately, make a patient question your expertise. These aren't reflections of your medical competence, but they are powerful factors in how a patient perceives you. For healthcare professionals looking to refine their delivery, understanding the role of accent reduction can be a significant step toward clearer dialogue. You can find more details here: https://intonetic.com/accent-reduction-for-professionals/doctors/
The Three Pillars of Effective Dialogue
To navigate these challenges, we'll focus on three foundational pillars that form the bedrock of successful patient interactions. Mastering these won't just protect your patients; it will also strengthen your professional credibility and make your job more rewarding.
- Clarity: Making sure your message is simple, direct, and free from confusing jargon.
- Empathy: Actively listening and responding to a patient's emotional state, so they feel truly heard and valued.
- Trust: Building a reliable, confident relationship where patients feel safe enough to share personal information and follow your guidance.
It's widely understood that effective communication in healthcare isn't just a nice-to-have skill. It’s the very foundation of patient safety, trust, and positive health outcomes. This guide will give you actionable strategies to strengthen each of these pillars.
Building a Foundation of Verbal Clarity
Everything a patient understands—or doesn't understand—starts the moment you open your mouth. You have the medical expertise, no question. But translating that knowledge into plain, clear English is what builds the bridge to patient trust and, ultimately, patient safety. This is especially true when English isn't your first language. Here, clarity is your single most powerful tool.
Let's be clear about one thing: this has nothing to do with having a "perfect" accent. It’s about making your message impossible to misunderstand. It means consciously simplifying complex ideas, nailing the pronunciation of critical terms, and using your voice to add that layer of meaning and reassurance patients need.
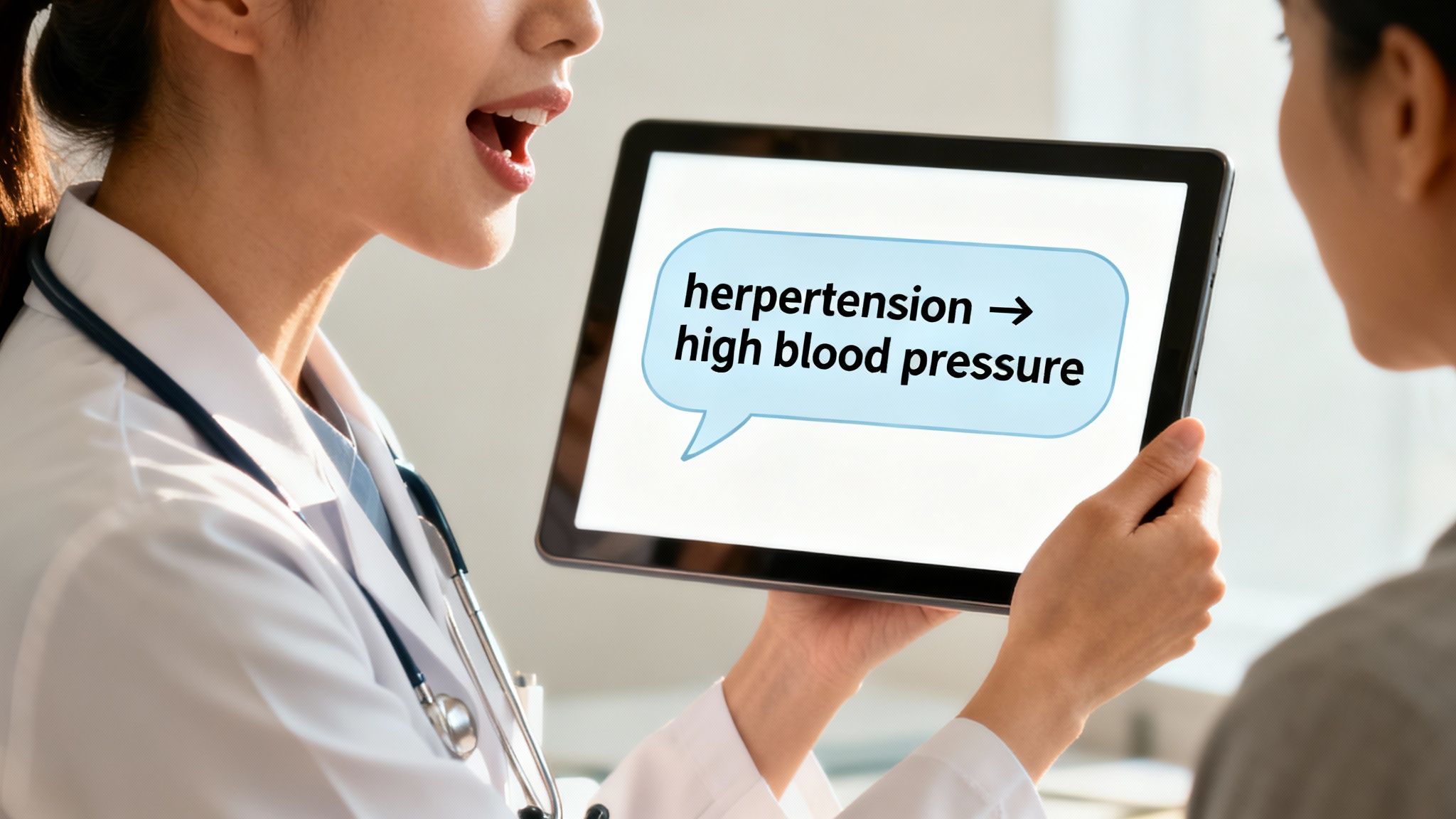
Swap Medical Jargon for Plain Language
We spend years learning the precise language of medicine, but to our patients, it might as well be a foreign language. A patient who is already feeling sick, scared, or overwhelmed is in no position to decipher unfamiliar terminology. The single fastest way to improve your communication is to trade clinical terms for simple, everyday words.
Think of yourself as a translator. Your job is to get the same essential information across without making the patient do the heavy lifting of figuring out what you mean. This one small shift can completely transform a patient’s experience from one of confusion to one of empowerment.
A survey of patients with chronic lymphocytic leukemia found a huge gap between what doctors thought they explained and what patients actually understood. In fact, only 54% of patients felt their questions were fully answered. That's a massive disconnect, and it highlights just how vital clear communication really is.
It’s a simple change in habit. Instead of saying, "The patient presents with acute myocardial infarction," you say, "The patient is having a heart attack." The second version is direct, eliminates any room for doubt, and ensures the seriousness of the situation is understood immediately.
Plain Language Alternatives for Common Medical Terms
Getting into the habit of using plain language takes a bit of practice. It's like building a new muscle. To help you get started, I've put together a quick-reference table for swapping out common medical terms for words your patients will instantly understand.
Keep this handy, and pretty soon, these translations will become second nature.
| Medical Term | Patient-Friendly Alternative | Example Sentence for Patient |
|---|---|---|
| Hypertension | High blood pressure | "Your blood pressure is higher than we'd like to see. The medical term for that is hypertension." |
| Myocardial Infarction | Heart attack | "The chest pain was caused by a heart attack, which means part of your heart muscle isn't getting enough blood." |
| Benign | Not cancerous | "The good news is that the growth is benign, which means it is not cancerous." |
| Malignant | Cancerous | "The test results show the tumor is malignant, so we need to discuss our plan for treating this cancer." |
| Edema | Swelling | "I see you have some edema in your ankles. That's just the medical term for the swelling you're experiencing." |
| Analgesic | Pain reliever | "I'm prescribing an analgesic to help with the discomfort. It's a type of pain reliever." |
| Tachycardia | Fast heart rate | "Your heart is beating much faster than normal right now, a condition we call tachycardia." |
The goal isn't to "dumb down" the information. It's about being respectful of your patient's state of mind and giving them information in a way they can actually use.
Master the Pronunciation of Critical Terms
Certain medical words can be a real mouthful, especially for non-native English speakers. While a slight accent is perfectly fine (and completely normal!), mispronouncing a key term can sometimes make a patient hesitate. It's not that they doubt your medical skills; it's that they might lose confidence in their own ability to understand your instructions correctly.
You don't need to master every word in the dictionary. Just focus on a small, core list of high-stakes words you say every day. Practice them. Break them down syllable by syllable and say them slowly until they roll off your tongue.
- Anesthesia: an-es-THEE-zha
- Cardiovascular: kar-dee-oh-VASK-yoo-ler
- Diabetes: dye-uh-BEE-tees
- Pulmonary: PULL-mon-air-ee
- Oncology: on-KOL-uh-jee
A great trick is to record yourself saying these words on your phone and listen back. It’s a surprisingly effective way to catch areas where you can improve. If you want to dive deeper, resources that teach you how to enunciate better can offer targeted exercises to really sharpen your pronunciation.
Use Intonation and Stress to Prevent Misunderstandings
How you say something is just as important as what you say. This is where intonation (the rise and fall of your voice) and sentence stress (emphasizing key words) become your best friends. They are crucial for adding meaning and making sure your instructions land exactly as you intend.
Think about this simple instruction: "Take this medication twice a day."
By punching the word "twice," you instantly signal that this is the most critical piece of information in the sentence. Without that emphasis, a distracted or anxious patient might just hear "take this medication a day" and miss the vital detail. A flat, monotonous delivery makes it incredibly hard for patients to sort vital commands from background noise.
Here’s a simple way to practice this:
- Find the Keyword: Before you speak, ask yourself: what is the one word in this sentence the patient absolutely cannot miss? It might be a number, a time, or a warning.
- Give it Emphasis: Make that keyword a little louder, a touch higher in pitch, or stretch it out just slightly.
- Use a Falling Tone for Commands: When giving an instruction, let your voice fall at the end of the sentence. This signals confidence and finality, which helps patients feel secure in your guidance.
Mastering these verbal skills isn't just about communication—it's about building a foundation of safety and trust with every single patient you see.
Connecting Through Empathy and Cultural Awareness
Once a patient can understand your words, the real work begins: making them feel understood as a person. This is where communication stops being a technical skill and becomes a true art. It's about moving beyond just clear speech and building a genuine human connection. This happens through empathy, active listening, and a real respect for cultural differences.
And this isn't just about being nice—it's a critical part of patient safety. A major systematic review in the Annals of Internal Medicine, which looked at 46 different studies, found something staggering. Poor communication contributes to 24% of all patient safety incidents and was the only cause in 10% of them.
When patients feel truly heard, they're far more likely to share vital information, stick to their treatment plan, and ultimately, trust your guidance.
The Power of Active Listening
Active listening is so much more than just waiting for your turn to talk. It's an engaged process. You have to hear what they're saying, process it, and then respond in a way that proves you were present with them. It’s all about putting the patient at the very center of the conversation.
Instead of just nodding along, try using reflective statements. This simple technique involves paraphrasing what the patient just told you, which both confirms your understanding and validates their feelings.
- Patient says: "I've been having this sharp pain in my chest, and I'm really scared it’s something serious."
- Your reflection: "It sounds like this chest pain is causing you a lot of worry, and you're concerned about what it might mean. Let's explore that together."
That simple rephrasing does two powerful things at once. It shows you've understood them correctly, and it acknowledges their emotional state, not just their physical symptoms.
Reading Beyond the Words
So much of what patients tell us is never actually spoken. Their body language, facial expressions, and tone of voice are a window into how they're really feeling. A patient might say, "I'm fine," while wringing their hands, avoiding eye contact, or speaking with a tremor in their voice.
Paying attention to these non-verbal cues is essential. If you notice a mismatch between their words and their actions, you can gently probe a little deeper.
"You've mentioned you're feeling fine, but I can see that you seem a little anxious. It’s completely normal to feel that way. Is there anything on your mind you'd like to share?"
This shows a deeper level of care. It gives the patient permission to open up about underlying fears they might have been hesitant to bring up themselves. And remember, your own body language is just as important. Keep an open posture, lean in slightly, and use appropriate eye contact. It all sends the message that you're engaged and approachable.
Navigating Cultural Sensitivities
Our patients come from countless cultural backgrounds, and each has its own set of norms around health, illness, and how to talk about them. What's considered respectful in one culture might be interpreted completely differently in another. This is where cultural awareness becomes the foundation of empathetic care.
A few examples I've seen in my own practice:
- Eye Contact: In many Western cultures, direct eye contact signals honesty. But in some Asian or Middle Eastern cultures, holding a gaze for too long, especially with an authority figure, can feel disrespectful.
- Directness: Some patients appreciate a direct, to-the-point style. Others, however, prefer a more gentle and indirect approach, especially when you're discussing a serious diagnosis or end-of-life care.
- Pain Expression: The way people show pain varies dramatically. Some are stoic and will actively downplay their discomfort, while others are much more vocal and expressive.
It's impossible to be an expert on every culture on the planet. The real key is to approach every single patient with humility and a genuine willingness to learn. You can ask open-ended questions like, "How is this kind of news usually discussed in your family?" or "What is most important to you as we make this decision?" This invites the patient to be your guide.
Understanding the impact of perceived differences, like how people react to different accents, is also part of this. You can learn more by exploring our guide on https://intonetic.com/what-is-accent-bias-understanding-the-hidden-workplace-challenge-for-non-native-speakers/.
To truly connect with patients and improve outcomes, you can also implement proven patient engagement strategies. When you combine these with empathetic listening and cultural humility, you build a foundation of trust that goes far beyond language and background, turning every interaction into an opportunity for healing.
Navigating Difficult Conversations with Confidence
Some of the most critical moments in healthcare don’t involve a procedure or a prescription; they happen during a conversation. Delivering difficult news, managing a frustrated patient, or simply ensuring complex instructions are fully understood are high-stakes situations that demand both skill and compassion.
Mastering these conversations is one of the most important parts of the job, turning challenging moments into opportunities to build real trust. This isn't just about handling edge cases. It's about being prepared for the inevitable, allowing you to remain professional and empathetic under pressure.
Confirming Understanding with the Teach-Back Method
One of the most powerful yet simple tools in my experience is the Teach-Back method. It’s a respectful way to check if a patient has truly understood what you've said, without making them feel like they're being quizzed.
The magic of this technique is how it shifts the responsibility from the patient's comprehension to your ability to explain. You're not asking, "Do you understand?" which almost always gets a quick "yes," even when they're lost.
By framing the check-in as a reflection of your own teaching, you create a safe, judgment-free space. You're not asking, "Did you get it?" but rather, "Did I do a good job explaining this?"
Here are a few prompts you can weave into your dialogue naturally:
- "I know this is a lot to take in at once. Just to make sure I explained it clearly, could you tell me in your own words how you'll take this medicine?"
- "We've covered the next steps. So we're on the same page, can you walk me through what you'll do when you get home?"
- "I want to be sure I did my part. Can you show me how you'll use the inhaler?"
This simple shift empowers patients and gives you immediate, honest feedback on whether your message truly landed.
Managing Frustration and Delivering Bad News
Handling a patient's anger, fear, or disappointment requires a different set of skills. When emotions are running high, the first step is always to de-escalate by acknowledging their feelings. Logic and explanations can wait; empathy has to come first.
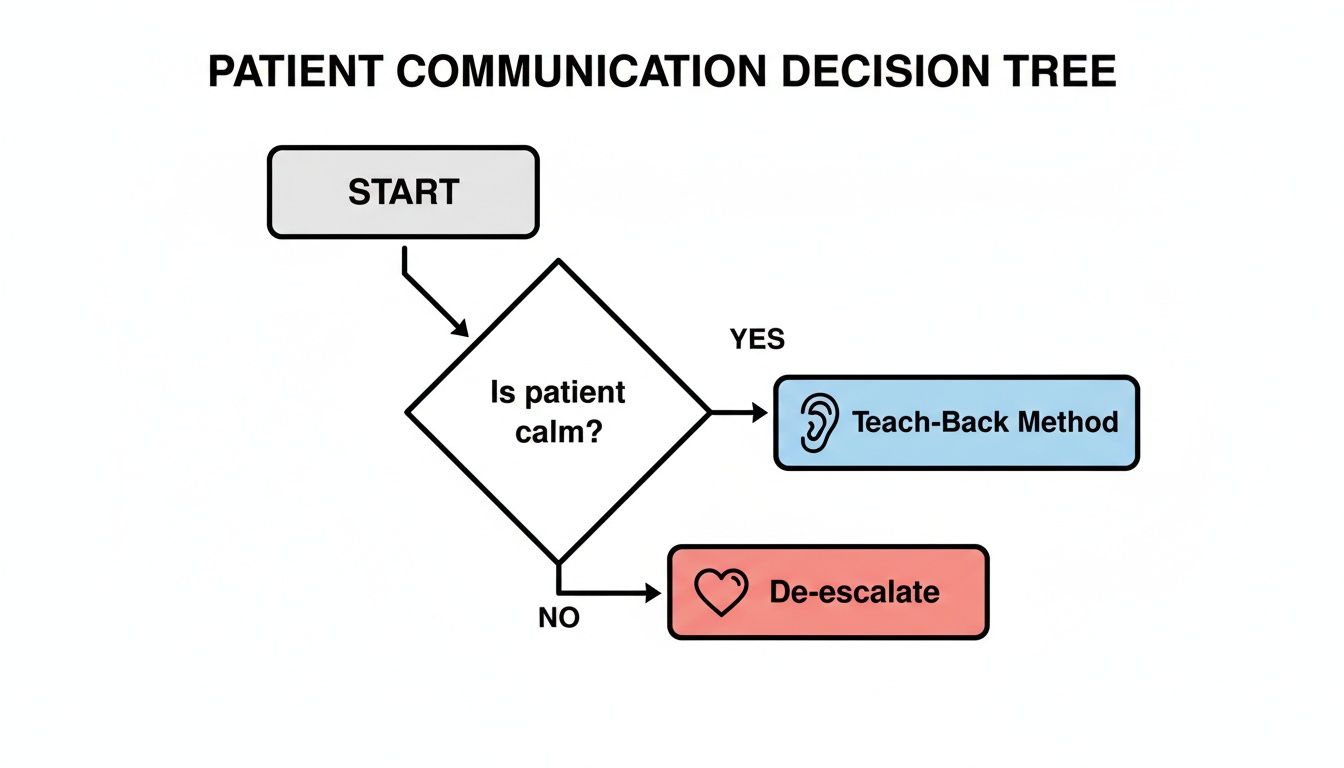
This decision tree gives you a simple visual guide for these high-stakes moments.
As you can see, the first step is always to assess the patient's emotional state. This tells you whether to use a clarifying tool like Teach-Back or shift immediately into de-escalation mode.
For those moments when you're facing an upset patient or delivering tough news, having a structured approach helps you maintain control while showing compassion.
The VALIDATE Framework for Difficult Talks
I recommend a simple framework to guide you. Think VALIDATE:
- Validate their feelings immediately. Show them you see their distress.
- Ask open-ended questions to understand their side of the story.
- Listen without interrupting. Let them get it all out.
- Identify the core problem from their point of view.
- Discuss potential next steps together. Make them part of the solution.
- Act on a mutually agreed-upon plan.
- Tell them you will follow up. This closes the loop.
- Empathize throughout the entire process. Never stop.
Here are a few short scripts that put this framework into action:
- For a frustrated patient: "I can see how upsetting this wait has been. Thank you for your patience. Let's look at what we can do right now to move things forward."
- When delivering bad news: "I have some difficult results to share with you. Before we go into the details, I want you to know we are here to support you every step of the way."
- Responding to a complaint: "It sounds like we didn't meet your expectations, and I am truly sorry for that. Can you tell me more about what happened so I can fully understand?"
These conversations are never easy, but having the right tools makes all the difference. Learning how to navigate these moments is a core reason professionals explore the top reasons to choose Intonetic for confident communication in high-stakes situations. By putting empathy first and always confirming understanding, you strengthen the patient-provider relationship when it matters most.
Adapting Communication for Telehealth and Digital Platforms
The way we connect with patients now extends far beyond the four walls of an exam room. Telehealth, patient portals, and even simple text messages have become standard practice, and this shift requires us to adapt how we communicate. When you're not physically in the room, the subtle cues of connection can easily get lost, making your verbal clarity more crucial than ever.
This move to digital isn't just a fleeting trend—it reflects a deep-seated patient preference. A 2021 survey revealed that a staggering 80% of patients want to use digital channels for at least some of their healthcare interactions. In fact, 44% prefer it most of the time. You can dig into the full report on these preferences over at Redpoint Global's website.
In this digital environment, clear, empathetic communication is non-negotiable. The safety net of in-person body language is gone, so your words and voice have to do all the heavy lifting.
Mastering the Virtual Exam Room
In a telehealth visit, your face and voice are your primary tools for building rapport and sharing vital information. You can't rely on a reassuring touch on the shoulder or observe a patient's full body language, which means you have to be much more intentional with your delivery.
Start by getting your setup right. A good microphone and a quiet, well-lit space are not just technical details; they are a sign of professionalism. They minimize distractions and show the patient they have your undivided attention.
When the screen is your only window to the patient, every word and vocal inflection carries more weight. Deliberate pacing, clear pronunciation, and intentional pauses become your most effective tools for building trust through the camera.
Next, you have to actively compensate for the distance. Lean in toward the camera slightly to show you're engaged. Use hand gestures, but make sure they're visible on screen. Most importantly, narrate what you're doing. Instead of a silent pause, say, “I’m looking closely at the picture of your rash now,” or, “I’m just taking a moment to review your chart on my other screen.” This kind of verbal signposting prevents awkward silences and keeps the patient right there with you.
Best Practices for Digital Communication
Clarity is just as vital when you're writing. Emails, portal messages, and texts are stripped of vocal tone, which means your words can be easily misinterpreted if you aren't careful.
- Be Clear and Concise: Get straight to the point. Short sentences and simple language are your best friends for conveying instructions or information.
- Set Expectations: If you're sending a message, let the patient know when to expect a reply. Something as simple as, "Our office will respond within one business day," makes a huge difference.
- Avoid Ambiguity: Before you hit send, read your message out loud. Does it sound friendly and professional? Could any part be misread as dismissive or, worse, alarming?
- Use Visual Aids: During video calls, the screen-sharing feature is your best friend. Use it to display lab results, diagrams, or medication schedules. Think of it as the digital equivalent of handing a patient a brochure—it can make a world of difference for their understanding.
These digital skills are now a core part of providing excellent patient care. For anyone looking to polish their on-screen presence, you might find our guide on how to speak more clearly on video calls really helpful. By tweaking your techniques for the digital world, you can make sure your communication stays effective, empathetic, and professional, no matter the platform.
Got a Question About Patient Communication?
Even with the best game plan, the day-to-day reality of patient care throws curveballs. We all have those moments. Mastering how to communicate with patients isn't a one-and-done task; it's something we refine over our entire careers. This section tackles some of the most common questions I hear from dedicated healthcare professionals, with quick, practical answers to help you handle these tricky situations with more confidence.
Think of this as your go-to guide for those "what do I do when…" moments.
How Can I Simplify Medical Information Without Sounding Condescending?
This is such a common and important concern. Nobody wants to come across as talking down to their patients. The secret is to frame the whole conversation as a partnership. Make it clear your goal is to be a great teacher, not to "dumb down" anything. Your patient's understanding is a direct reflection of how well you explain things.
One of the best ways to do this is with simple, everyday analogies. For example, instead of getting deep into the pathophysiology of arterial plaque, you could say, "Think of this artery like a plumbing pipe in your house that's slowly getting clogged. Our job is to clear that blockage so everything can flow freely again."
It’s a simple picture, but it works.
After you've simplified a concept, the next step is crucial. You have to check for understanding in a way that puts the responsibility back on you.
- "Does that comparison make sense to you?"
- "I know I just threw a lot of information at you. What parts are still a little fuzzy?"
- "Just to be sure I did a good job explaining, can you tell me in your own words what you'll do when you get home?"
That last one is the heart of the Teach-Back method, and it's incredibly powerful. It shifts the focus from testing their intelligence to checking your clarity as an educator. This creates a safe space for them to admit they're confused and ask for help.
What's the Best Way to Talk to a Patient Who Is Angry or Upset?
When a patient is emotional, your first job isn't to solve the problem—it's to de-escalate the emotion. Someone who is angry or overwhelmed can't process information or think logically. Your immediate response has to be grounded in empathy.
First, take a breath. Stay calm and just listen. Don't interrupt, and don't get defensive, even if you feel you're being unfairly blamed. Let them get it all out. Acknowledging their feelings is the single most important thing you can do.
"I can see how frustrating this is for you, and I really want to understand what happened. Please tell me more."
That simple statement validates their experience. It shows you're on their side, not against them. Once they've finished, try paraphrasing their main points back to them.
For example: "Okay, so if I'm hearing you right, you're upset about the long wait and the fact that no one gave you an update." This proves you were actually listening and gives them a chance to correct you. Only after they feel heard and understood can you start working together on a solution.
I Worry My Accent Makes Me Seem Less Authoritative. How Can I Build Trust?
This is a fear I hear from so many skilled, non-native English-speaking professionals. But it's so important to separate accent from authority. True authority in a clinical setting doesn't come from a specific accent—it comes from clarity, confidence, and competence. Patients trust you when they understand you easily and feel secure in your guidance.
So, let's shift the focus to the things you can absolutely control.
- Precise Pronunciation: Nail the key medical terms. When words like "anesthesia" or "oncology" come out of your mouth with precision, it immediately signals expertise.
- Logical Intonation: When you give instructions or state a fact, end your sentences with a falling tone. It’s a subtle vocal cue that naturally conveys confidence and finality, which is very reassuring for a patient.
- Deliberate Pacing: Just slowing down a little bit can make a world of difference in how well you're understood. Rushing can sound like nervousness, but a steady, deliberate pace signals thoughtfulness and control.
When you know, deep down, that patients can understand you the first time, your delivery will naturally become more authoritative. Trust is built on clear communication, and a confident, easy-to-understand message is far more powerful than any accent.
At Intonetic, we help healthcare professionals master the nuances of clear, confident speech. Our coaching is all about giving you control over your pronunciation, intonation, and rhythm, so you're always understood the first time. Build unshakeable patient trust by booking your free assessment today.