Effective communication in healthcare: Key skills for safer patient outcomes
Effective communication in healthcare isn’t just about exchanging information; it’s about making sure that information is clear, accurate, and delivered with empathy between clinicians, patients, and their families. It’s a fundamental clinical skill that directly impacts patient safety, cuts down on medical errors, and builds the trust you need for positive health outcomes.
Why Communication Is a Critical Clinical Skill

We’ve all seen it happen. A patient leaves the clinic after a rushed, five-minute consultation. They’re holding a new prescription, but they’re not really sure why they need it, how it interacts with their other meds, or what side effects to watch for. This scenario is far too common, and it points to a massive gap: even the sharpest medical expertise falls flat if it isn’t communicated well.
For too long, communication has been brushed off as a “soft skill.” But in reality, it’s a core clinical competency, every bit as vital as diagnosing an illness or performing a procedure. When communication breaks down, patient safety is compromised, trust disappears, and the best-laid care plans fall apart.
The stakes—both financial and personal—have never been higher. Recent global surveys show that 84% of healthcare consumers say quality communication is essential to their experience. Even more telling, a staggering 69% are likely to switch providers simply because of poor communication.
Moving Beyond Theory to Action
This guide is designed to move you past abstract ideas and into actionable techniques you can use immediately to master effective communication. We’ll dig into structured frameworks, verbal delivery tactics, and strategies that work across diverse settings.
For non-native English-speaking professionals, this focus on clarity is especially crucial. Finding the right support, like the https://intonetic.com/whos-the-best-accent-reduction-coach-for-healthcare-workers-in-english-speaking-countries/, can be a huge step in building the confidence needed to connect with every patient.
Communication is the single most critical component of delivering safe, high-quality, and patient-centered care. It’s the foundation upon which every other clinical action is built.
To make things even more efficient, many teams are now integrating advanced tools like voice recognition software for healthcare. This technology can make a real difference in patient care by streamlining documentation and minimizing errors, freeing you up to focus on the conversation.
Core Pillars of Effective Clinical Communication
To give you a clear roadmap of what’s ahead, this table breaks down the core pillars we’ll be covering in this guide. Think of it as a quick-glance summary of what you’ll learn and why it’s so important for your practice.
| Pillar | Core Concept | Key Benefit |
|---|---|---|
| Structured Frameworks | Using evidence-based models like SBAR and teach-back to standardize communication. | Reduces medical errors and ensures critical information is conveyed accurately. |
| Verbal & Non-Verbal Delivery | Mastering tone, pace, and body language to build rapport and convey empathy. | Increases patient trust, comprehension, and adherence to treatment plans. |
| Adapting for Diverse Settings | Tailoring communication for telehealth, cross-cultural interactions, and interpreters. | Ensures equitable, effective care for all patients, regardless of background or setting. |
| Personal Improvement Plan | Implementing continuous self-assessment, peer feedback, and structured practice. | Turns communication into a practiced, reliable skill that improves over time. |
By mastering these pillars, you can transform your patient interactions from simple information exchanges into powerful tools for building trust and improving health outcomes. Let’s dive in.
Using Structured Frameworks to Reduce Errors
In a high-stakes clinical setting, ambiguity is the enemy. When you’re relying on memory or improvising during a critical patient handoff, you’re introducing unnecessary risk. This is where structured communication frameworks come in. They provide a shared mental model for the entire team, making sure vital information gets across clearly, concisely, and completely—every single time.
Think of these frameworks not as rigid scripts meant to stifle your clinical judgment, but as safety tools, just like a surgical checklist. They create a predictable, reliable format for exchanging information, which is an absolute lifesaver during stressful situations or when you’re working with new team members.

Mastering the SBAR Framework for Clear Handoffs
One of the most effective tools I’ve seen in practice is SBAR, which stands for Situation, Background, Assessment, and Recommendation. It’s a simple framework that brings order to conversations that could easily become rambling and confusing, especially during those crucial nurse-to-doctor calls.
Here’s how it works:
- Situation: A quick, punchy statement of the immediate problem. What’s happening right now that needs attention?
- Background: Just the essential context. What’s the patient’s diagnosis, relevant history, and recent treatments?
- Assessment: Your professional conclusion. What do you think is going on?
- Recommendation: Your specific request. What do you need from the person you’re calling?
A common pitfall is giving too much background upfront, burying the urgent situation in a sea of details. Another classic mistake is having a weak or non-existent recommendation, leaving the other clinician guessing what you need from them.
The real power of SBAR lies in its focus on action. It shifts the conversation from just reporting a problem to actively proposing a solution, empowering every team member to contribute to patient safety.
Let’s walk through a real-world example of a nurse calling a physician about a post-op patient.
Poor Communication (Without SBAR):
“Hi Dr. Evans, this is Sarah from the surgical floor. I’m calling about Mr. Thompson in room 204. He had his knee replacement this morning and he’s been complaining of some pain, and his heart rate has been a little high. I just wanted to let you know.”
This leaves Dr. Evans with more questions than answers. How urgent is this? What does Sarah actually need?
Effective Communication (Using SBAR):
- Situation: “Hi Dr. Evans, this is Sarah. I’m calling about Mr. Thompson in room 204. He is experiencing acute shortness of breath and chest pain.”
- Background: “He is a 68-year-old male, post-op day one from a total knee replacement. He has no prior cardiac history, but his heart rate has been sustained in the 120s for the last hour.”
- Assessment: “I am concerned he may be having a pulmonary embolism.”
- Recommendation: “I recommend you come see him immediately. In the meantime, should I order a STAT EKG and apply oxygen?”
This version is direct, clear, and provides an actionable plan. This kind of structured approach doesn’t just improve safety; it builds mutual respect among team members. For teams looking to hone these skills, it’s worth exploring our blog on how to use role playing and simulation exercises for speech improvement.
Using Teach-Back to Confirm Patient Understanding
While SBAR streamlines clinician-to-clinician handoffs, the teach-back method is absolutely essential for making sure patients and their families truly understand their care plan. It’s a simple but profound technique that flips the script, placing the responsibility for clear communication on the provider, not the patient.
The goal isn’t to quiz the patient. It’s to confirm how well you did at explaining the information.
Instead of asking a closed-ended question like, “Do you have any questions?” (which almost always gets a “no”), you use open-ended prompts. This gives patients a chance to explain their understanding in their own words. To improve accuracy here, it’s interesting to see how innovations like Healthcare Documentation Automation can also serve as valuable structured frameworks for preventing communication errors.
Here are a few of my go-to teach-back prompts:
- “We’ve gone over a lot today. To make sure I did a good job explaining everything, can you tell me in your own words how you’re going to take this new medication when you get home?”
- “I want to be sure we’re on the same page. What are some of the important side effects we talked about that would make you want to call our office?”
- “Just to check my explanation, could you show me how you’ll use the inhaler?”
If a patient’s explanation is off, it’s not their failure—it’s your cue to explain it again, maybe in a different way. You can say, “Thanks for sharing that. I think I may have confused you on one part. Let me try explaining it another way.” This collaborative approach turns patient education from a one-way lecture into a real conversation, which makes a world of difference for adherence and safety.
Fine-Tuning Your Verbal and Non-Verbal Delivery
If your clinical framework is the skeleton of a good patient interaction, then your delivery—how you actually speak and carry yourself—is what brings it to life. Your words are just one piece of the puzzle. The subtle, often unconscious, verbal and non-verbal signals you send can either build a bridge of trust or throw up a wall of confusion.
Getting these elements right is a cornerstone of effective communication in healthcare. It’s about making sure patients don’t just hear the words, but they also feel the empathy and reassurance behind them. This is especially true when you’re working with people who have low health literacy, where your clarity and tone can make all the difference in their ability to understand and follow through.
Simplifying Medical Language Without Being Patronizing
One of the biggest hurdles we face in patient communication is what’s known as the “curse of knowledge.” As clinicians, we’re so immersed in medical terminology that it’s easy to forget that words like “hypertension,” “prophylactic,” or “adverse effects” sound like a foreign language to most patients. The trick is to simplify this language without sounding condescending.
Instead of just swapping jargon for simpler terms, try using analogies that connect to a patient’s everyday life.
- Instead of: “We need to titrate your dose of this antihypertensive medication.”
- Try: “We need to find the exact right amount of this blood pressure medicine for you, kind of like finding the perfect volume on a radio dial. We’ll start low and adjust it slowly until it’s just right.”
This approach respects the patient’s intelligence while making the information accessible and far more memorable. It shifts the dynamic from a top-down directive to a collaborative partnership.
The goal isn’t to “dumb down” the information. It’s to translate it into a language the patient already speaks fluently. True clarity is a sign of expertise, not a simplification of it.
Using Intonation to Convey Empathy and Importance
Your tone of voice can say so much more than your words. A flat, rushed tone can make a patient feel like another task to be checked off, while a warm, measured tone communicates genuine compassion and presence. Intonation, the natural rise and fall of your voice, is a powerful tool for building that connection.
For instance, when delivering difficult news, a slightly lower pitch and slower pace can communicate gravity and compassion. On the flip side, when explaining a positive step in their care plan, a slightly more upbeat and varied intonation can instill confidence and hope.
Stressing Key Words for Maximum Impact
In any sentence, some words carry more weight than others. By consciously adding stress—a little more volume or holding a word for a fraction longer—you can guide the patient’s focus to the most critical information. This is a game-changer for instructions and warnings.
Think about this instruction: “It is very important that you take this medication with food.”
Said flatly, the message can get lost in the shuffle. But by emphasizing the key parts, you create instant clarity:
“It is very important that you take this medication with food.”
That small change is like taking a verbal highlighter to the most critical action, which can significantly boost the chances of adherence. The same logic applies to side effects: “If you experience any shortness of breath, you need to call us immediately.”
Finding the Right Conversational Rhythm and Pace
When we get busy, our speech naturally speeds up. For patients who are already anxious or trying to absorb complex information, this rapid-fire delivery can be completely overwhelming. A rushed pace signals impatience and can shut down the conversation, making patients hesitant to ask the very questions they need answered.
The best way to counter this is to consciously pause. After you explain a key concept, just stop for a few seconds. This gives the patient a moment to process what you’ve said and formulate a question. It turns your monologue into a dialogue and shows that you genuinely care about their understanding.
A great way to check your own delivery is to record yourself explaining a common medical concept. Listen back and pay attention to your pace, your tone, and how you use pauses. For anyone looking for more structured guidance, there are fantastic resources that explain how to enunciate better and offer practical exercises to improve your clarity and delivery. Mastering these subtle aspects of speech will make your communication far more effective and truly patient-centered.
Adapting Communication for Diverse and Digital Settings
Effective communication in healthcare today reaches far beyond the four walls of an exam room. The modern clinical landscape is a dynamic mix of different cultures, languages, and, increasingly, digital platforms. Being able to navigate this complexity isn’t just a “nice-to-have” skill—it’s absolutely essential for providing equitable care and building the kind of patient trust that leads to better outcomes.
Let’s be clear: adapting your style is a clinical necessity. A communication strategy that works perfectly for one patient might fall completely flat with another, whether due to deep-seated cultural differences or the impersonal nature of a screen. The key is to stay flexible, observant, and intentional in every single interaction.
Navigating Cross-Cultural Conversations with Sensitivity
Working with patients from diverse backgrounds demands more than just top-notch clinical skills; it requires a genuine sense of cultural humility. This means recognizing that your own cultural lens isn’t universal and making an active effort to understand the patient’s world. It’s the small, unconscious assumptions that can quickly erode trust.
For instance, in some cultures, making direct eye contact is a sign of respect and attentiveness. In others, it can be interpreted as aggressive or confrontational. The role of family in medical decisions also varies dramatically. Some patients will expect their entire family to be part of a consultation, while others would be horrified at the idea of discussing their health so publicly.
When language barriers pop up, using a professional medical interpreter is non-negotiable. It’s a common but dangerous mistake to rely on a patient’s family member, especially a child. They often lack the medical vocabulary to translate accurately and may feel pressured to soften difficult news, which can create critical, even life-threatening, gaps in understanding.
A patient’s cultural background profoundly shapes their beliefs about illness, treatment, and authority. The best clinicians don’t just treat a condition; they treat a person within their cultural context, showing deep respect for their values and beliefs.
Best Practices for Working with Interpreters
To get the most out of these sessions, a few key guidelines make all the difference:
- Speak directly to the patient, not the interpreter. Your connection is with the patient, so maintain eye contact with them to build that crucial rapport.
- Use short, simple sentences and pause often. This gives the interpreter time to convey your message accurately without having to memorize long, complex explanations.
- Ditch the medical jargon and idioms that don’t translate well. Instead of saying something like “it’s a long shot,” be direct and say, “it is unlikely to work.”
- Always allow extra time for the appointment. A conversation that flows through an interpreter will naturally take longer than a direct one.
Following these simple rules can transform a clumsy three-way conversation into a smooth, patient-centered dialogue.
Mastering the Virtual ‘Webside Manner’ in Telehealth
The massive shift toward digital health has rolled out a whole new set of communication challenges. Building rapport and conveying empathy through a screen requires a much more deliberate approach than you might use in person. We’re seeing growing frustration with clunky digital experiences, and patients are increasingly putting a premium on convenience.
In fact, 65% of patients now see virtual health as more convenient than trekking to an in-person visit, a preference that has only solidified in recent years. To meet this demand without sacrificing care quality, we have to adapt. You can read more about what patients are looking for in the state of healthcare communication on MedicalEconomics.com.
Your virtual presence, or ‘webside manner,’ is make-or-break. Start with your tech setup. Position your camera at eye level to mimic direct eye contact—a simple stack of books can work wonders. Make sure your lighting is good and your background is professional and free of distractions.
During the actual call, your verbal and non-verbal cues carry even more weight. Since you can’t rely on the subtle body language of an in-person visit, you have to be more explicit.
- Use verbal nods: Simple phrases like “I see,” “That makes sense,” or “Tell me more about that” are powerful. They reassure the patient you are locked in and listening.
- Summarize what you hear, often: Pause the conversation and say something like, “Okay, so what I’m hearing is that the pain is sharpest in the morning. Is that correct?” This confirms you understand and shows you’re engaged.
- Mind your expressions: A warm, attentive facial expression can go a surprisingly long way in building trust through a screen.
For any clinician looking to polish their on-screen presence, our guide on how to speak English more clearly on video calls offers specific, actionable techniques to make sure your message always lands perfectly.
To help visualize the different tactics needed for these settings, here’s a quick comparison of the bedside versus the telehealth approach.
Bedside vs. Telehealth Communication Strategies
| Communication Element | In-Person (Bedside) Approach | Telehealth Approach |
|---|---|---|
| Non-Verbal Cues | Rely on natural body language, gestures, and physical proximity to build rapport. | Use exaggerated facial expressions, deliberate nods, and hand gestures that are visible on camera. |
| Building Rapport | Can be established through a handshake, a comforting touch on the arm, and shared physical space. | Requires an intentional warm-up period, direct eye contact with the camera, and an engaged tone of voice. |
| Active Listening | Demonstrated through eye contact, leaning in, and subtle facial expressions. | Needs explicit verbal affirmations (“I see,” “Go on”) and frequent summaries to confirm understanding. |
| Patient Education | Use physical models, printed handouts, and drawing on whiteboards to explain concepts. | Utilize screen sharing for diagrams, send digital resources via chat, and use clear, simplified language. |
| Managing Silence | Pauses can feel natural and allow for reflection. | Awkward silences can be mistaken for tech issues; narrate actions (“I’m just pulling up your chart now”). |
Ultimately, whether you are at the bedside or on a video call, the core principles of clear communication remain the same. The environment changes, but the goal of connecting with the patient doesn’t.
This infographic breaks down four foundational principles that are critical in any conversation, in-person or digital.
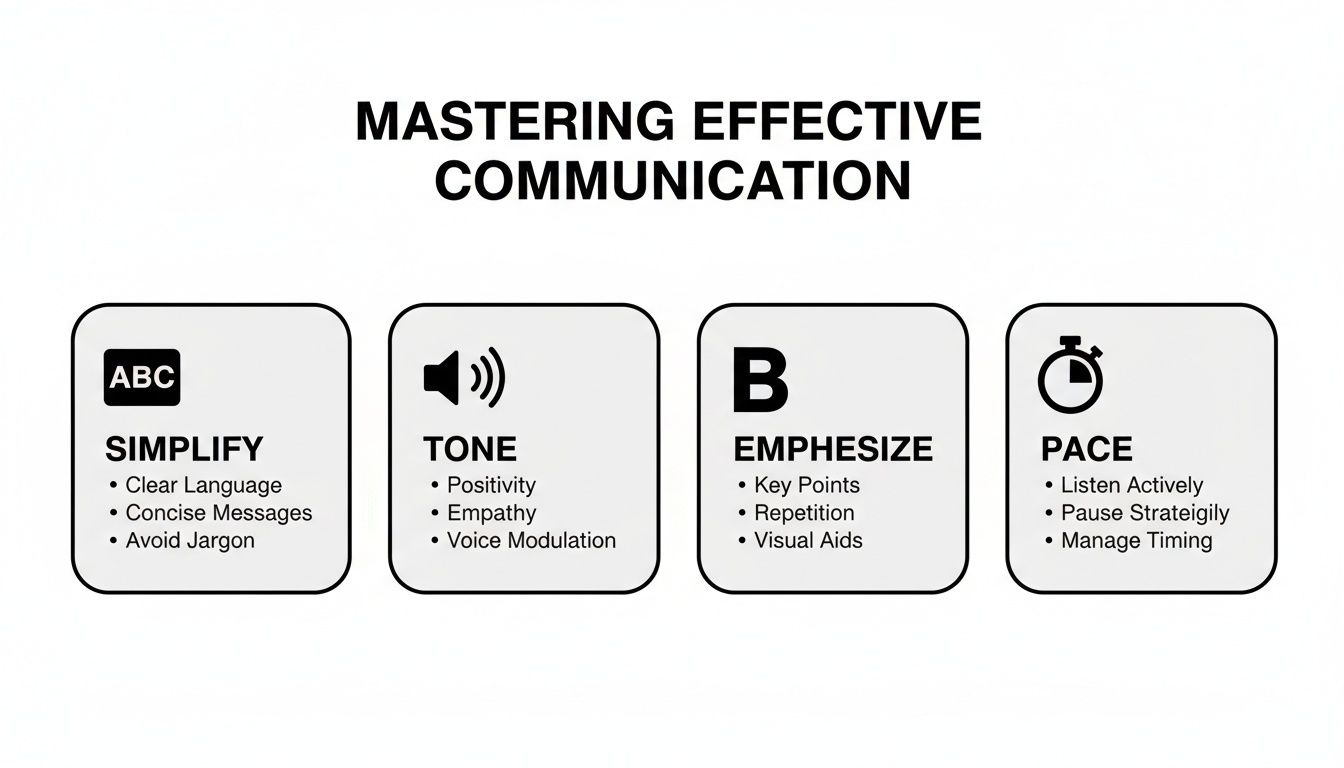
Truly mastering these four elements—simplifying your language, controlling your tone, emphasizing what matters most, and managing your pace—is the bedrock of clear, effective communication in any healthcare setting you find yourself in.
Creating Your Personal Communication Improvement Plan
Mastering clear, effective communication in a clinical setting isn’t a one-and-done course you take. Just like any other clinical skill, it’s a muscle that requires ongoing practice, reflection, and refinement. The best way I’ve seen clinicians turn good intentions into real, sustainable habits is by creating a personal improvement plan.
This isn’t about piling more tasks onto your already overflowing plate. It’s about weaving small, intentional practices into the work you’re already doing. The real goal here is to build a habit of reflection—where you consistently check in on your skills, pinpoint areas for growth, and actively work on new techniques until they feel like second nature.
The healthcare industry as a whole is catching on. Market analysts are projecting the global healthcare communications sector to skyrocket to $43.26 billion by 2032. This is a powerful signal that organizations are finally investing serious resources into building trust and clarity. You can dive deeper into this trend in the full healthcare marketing communications industry outlook on BusinessWire.com.
Starting With Self-Assessment and Feedback
The journey to better communication always starts with an honest look in the mirror. This doesn’t have to be complicated. It can be as simple as taking two minutes after a tricky patient conversation to ask yourself: What went well? What could I have made clearer? Did they truly seem to understand their care plan, or were they just nodding along? Did my teach-back actually work?
Peer feedback is another incredibly powerful tool, but it requires a foundation of trust and psychological safety. When colleagues feel safe enough to share constructive observations, everyone wins.
- Find a trusted colleague and agree to observe each other for a week, maybe during a patient handoff or a family meeting.
- Give specific, actionable feedback. Instead of a vague “That was a bit confusing,” try something like, “Next time, maybe we could try explaining the side effects before getting into the dosage schedule. I think it might land better.”
- Receive feedback with grace. Thank your colleague for taking the time. See it as valuable data for your improvement plan, not a personal jab.
Continuous improvement isn’t about being perfect. It’s about being a little better today than you were yesterday. Every single interaction is a fresh opportunity to practice and refine your approach.
Designing Your Structured Practice Plan
Once you’ve identified a few areas for growth, you can build a simple, structured plan. The secret is to avoid overwhelming yourself by focusing on just one specific skill at a time. This is a classic skill-acquisition strategy that helps build muscle memory and true confidence.
For clinicians working on their pronunciation and clarity, it’s incredibly helpful to learn how to set micro-goals to stay on track with the journey. Breaking a big goal down into small, weekly targets makes it feel much more manageable and keeps you motivated.
Here’s a sample four-week plan you can easily adapt for your own goals:
| Week | Focus Area | Practice Activity |
|---|---|---|
| Week 1 | Mastering Teach-Back | Use a teach-back prompt in at least three patient interactions each day. Keep a note of which phrases seem to work best. |
| Week 2 | Clarity in SBAR Handoffs | Before every handoff, jot down one key bullet point for each SBAR category. Time yourself to keep the report under two minutes. |
| Week 3 | Improving Vocal Tone | Record yourself on your phone explaining a common diagnosis. Listen back just for your tone and pace. Do you sound reassuring? Rushed? |
| Week 4 | Cross-Cultural Sensitivity | In a team huddle, role-play a scenario that involves an interpreter. The key is to practice speaking directly to the patient, not the interpreter. |
This kind of structured approach transforms a vague ambition like “get better at communication” into a concrete set of actions. By homing in on one small skill each week, you create a powerful cycle of practice, reflection, and growth that will have a real, lasting impact on your clinical practice.
Your Questions, Answered
I get it. Even with the best intentions, trying to weave new communication habits into an already chaotic clinical workflow feels like one more thing to do. It’s one thing to understand the idea behind SBAR or teach-back, but another thing entirely to pull it off during a hectic shift.
Let’s tackle some of the most common questions I hear from clinicians. My goal here is to bridge that gap between knowing what to do and feeling confident actually doing it. These are real-world concerns, and the answers are designed to be simple, effective, and easy to fold into your daily practice.
How Can I Actually Use SBAR When My Shift Is a Mess?
The trick to making SBAR work when you’re slammed is to take 30 seconds to prepare. I know, it feels counterintuitive to stop when you’re rushing, but this tiny bit of prep saves you minutes of confusing back-and-forth later. Before you even think about picking up the phone, grab a sticky note.
Jot down a single, quick bullet for each letter:
- S (Situation): “Mr. Chen, Rm 302, BP dropped to 85/50.”
- B (Background): “Post-op day 2 colectomy, on IV fluids.”
- A (Assessment): “I think he’s going septic.”
- R (Recommendation): “Need you to see him now. Start a fluid bolus?”
This little cheat sheet turns a potentially rambling, stressful call into a focused, two-minute exchange. The structure is the time-saver. It forces you to get straight to the point and anticipates the questions you’re about to be asked. Some of the sharpest units I’ve seen have even started printing little SBAR notepads to make this second nature.
What if a Patient Gets Annoyed with the Teach-Back Method?
This is a huge—and completely valid—concern. Patients get frustrated with teach-back when it feels like a test. If they think you’re quizzing them, their defenses go up immediately.
The key is all in how you frame it. You have to shift the burden from their ability to learn to your ability to teach.
Never say something like, “Okay, I want to see if you understood that.” That language puts all the pressure on them.
Instead, make it about checking your own performance.
“I want to be sure I did a good job explaining this. Could you walk me through how you’ll take this medicine when you get home, just so I know I was clear?”
See the difference? You’re making the patient your partner in confirming your communication was effective. It’s no longer a pop quiz; it’s a collaborative effort to ensure their safety. This tiny change in wording completely transforms the dynamic.
Are There Any Quick Fixes for Better Telehealth Communication?
You bet. You can make a huge difference in your virtual visits with just a few small tweaks, and you can start today. Think of these three things as your “webside manner” essentials—they build trust and connection right through the screen.
- Get Your Camera Angle Right. Position your camera at eye level. Use a stack of books, a laptop stand, whatever it takes. This tiny change creates the feeling of direct eye contact and makes you seem far more engaged.
- Acknowledge the Elephant in the Room (The Tech). Kick off the call by addressing the medium itself. A simple, “Hi there, can you see and hear me okay? Just give me a heads-up if the connection gets choppy,” builds instant trust and shows you get the limitations of the technology.
- Narrate What You’re Doing. Non-verbal cues are tough to catch on video, so you have to be more obvious. Use frequent verbal nods and summaries. Little phrases like, “Okay, so what I’m hearing is the pain is worse in the morning…” or “That makes sense” reassure the patient you’re not just staring at a screen—you’re actively listening.
These adjustments are small, but they add up fast. They help shrink that digital distance, making patients feel seen and heard, even when you’re miles apart. Mastering these details is a cornerstone of effective communication in healthcare, no matter the setting.
At Intonetic, we help non-native English-speaking healthcare professionals communicate with the clarity and confidence their clinical skills deserve. If you’re ready to make sure you’re understood the first time, every time, see how our personalized accent coaching program can help.

